Endocannabinoid System and Immune System
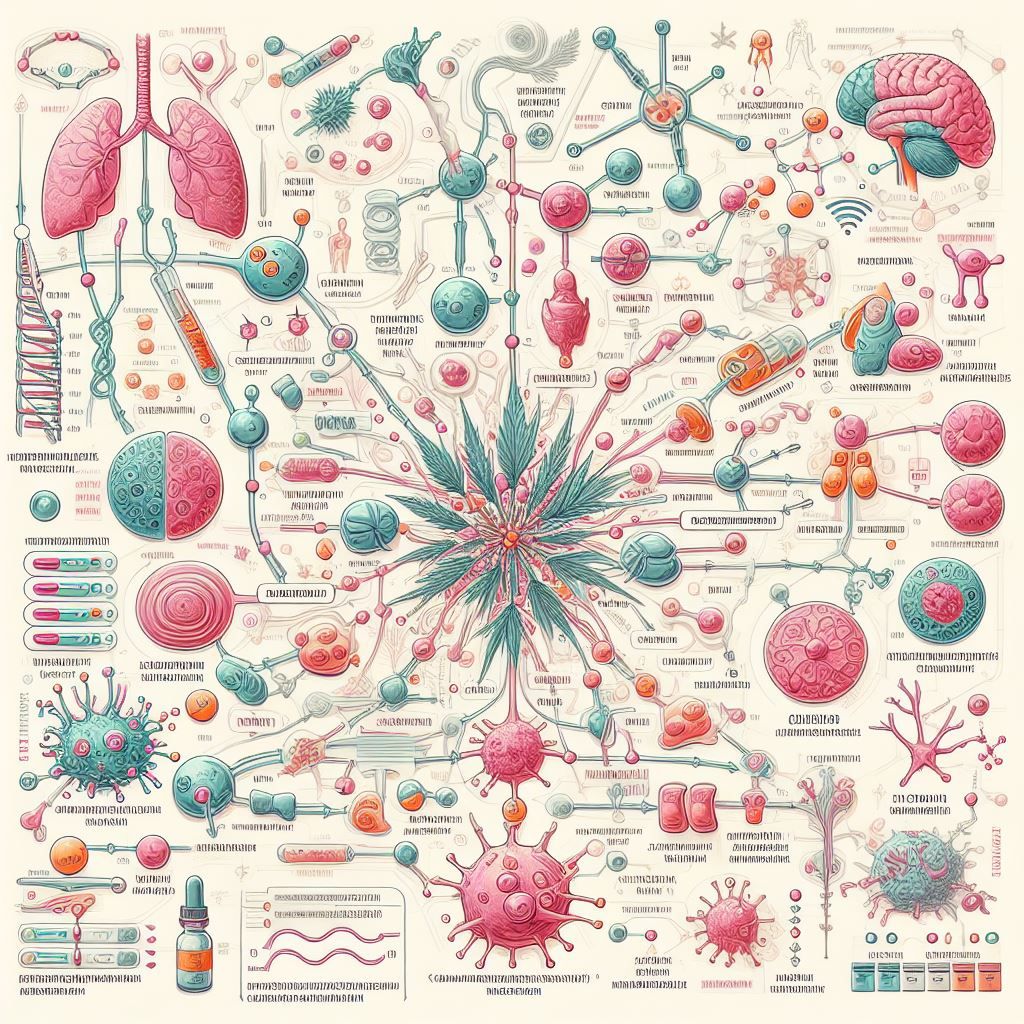
Examining the Intricate Link Between the Endocannabinoid System and Immune System: An Extensive Guide
Introduction to the Endocannabinoid System (ECS)
The endocannabinoid system (ECS) is a complex cell-signaling system that plays a critical role in regulating a variety of physiological processes. At its core, the ECS consists of endocannabinoids, cannabinoid receptors, and enzymes that synthesize and degrade endocannabinoids.
Overview of ECS components
Endocannabinoids are endogenous lipid-based neurotransmitters produced on demand by cells in the brain and body. The two main endocannabinoids are anandamide and 2-AG (2-arachidonoylglycerol). These endocannabinoids bind to and activate cannabinoid receptors found throughout the central and peripheral nervous systems. There are two primary cannabinoid receptors that mediate the effects of endocannabinoids:
- CB1 receptors: Primarily found in the central and peripheral nervous systems
- CB2 receptors: Mainly expressed on immune cells and tissues
Enzymes regulate endocannabinoid levels through synthesis or degradation. For example, fatty acid amide hydrolase (FAAH) breaks down anandamide, while monoacylglycerol lipase (MAGL) metabolizes 2-AG.
Significance of the ECS
The ECS has emerged as a key player in modulating major physiological systems:
- Appetite and digestion
- Pain perception
- Mood and motivation
- Memory and learning
- Inflammatory and immune responses
In essence, the ECS functions like a dimmer switch, fine-tuning many biological processes to maintain homeostasis. Dysregulation of the ECS has been implicated in multiple diseases, underscoring its broad influence throughout the body.
The ECS and Immune System Connection
The endocannabinoid system (ECS) plays a critical role in regulating immune cell function and maintaining homeostasis. This has led to the concept of an 'immuno-cannabinoid system' - an intersection between the ECS and immune system.

Role of the ECS in Immune Regulation
Endocannabinoids like anandamide and 2-AG modulate several aspects of both innate and adaptive immunity. They influence T- and B-lymphocyte proliferation, apoptosis (programmed cell death), and the production of inflammatory cytokines
- Anandamide suppresses T-cell proliferation and induces apoptosis in activated, but not naive T-cells
- 2-AG stimulates the migration of B-cells and macrophages towards sites of inflammation
Through these effects, the ECS fine-tunes immune responses, preventing excessive inflammation on one hand and improper immune activation on the other. This helps maintain homeostasis.
Modulation of Inflammatory Mediators
The ECS also regulates the immune system by modulating inflammatory mediators like cytokines. Endocannabinoids limit inflammatory cytokine production by immune cells. For example, anandamide suppresses IL-2 secretion by activated T-lymphocytes. The ECS also stimulates anti-inflammatory cytokines like IL-10. Furthermore, endocannabinoids regulate immune cell migration towards inflamed tissues by modulating chemokines.
- Decreasing pro-inflammatory chemokines
- Increasing anti-inflammatory chemokines
Through these synergistic mechanisms, the ECS prevents excessive immune activation and tissue damage due to uncontrolled inflammation. Proper ECS tone is therefore critical for optimal coordination between the nervous, endocrine and immune systems. Dysregulation of this delicate balance can trigger disorders like autoimmunity, allergies and chronic inflammatory conditions. Modulating the ECS shows promise as a therapeutic strategy for such immune-mediated diseases.
Cannabinoid Receptors in Immune Function
The endocannabinoid system interacts with the immune system primarily through two main receptors - CB1 and CB2. These receptors are expressed on various immune cells and modulate several aspects of immune function.
Differential Expression of CB1 and CB2 Receptors
CB1 receptors are predominantly expressed in the central and peripheral nervous systems. In contrast, CB2 receptors are mainly found on immune cells such as T cells, B cells, macrophages, neutrophils, and natural killer cells. This differential expression allows the endocannabinoid system to exert distinct regulatory effects - CB1 mediates neurological functions while CB2 modulates immune responses.
Role of CB2 Receptors in Immune Cell Function
Activation of CB2 receptors influences several key immune processes:
- Regulates immune cell migration towards sites of inflammation and infection
- Modulates cytokine production and release from activated immune cells
- Influences T cell and B cell proliferation and differentiation
- Mediates apoptosis in activated immune cells
Through these mechanisms, CB2 receptor signaling helps resolve inflammatory responses and maintain immune homeostasis. Selectively targeting CB2 may thus hold therapeutic potential for inflammatory and autoimmune conditions without causing psychotropic effects.
B Cell Function and CB2 Receptors
An emerging area of research is the role of CB2 receptors in regulating B cell responses. Studies show CB2 activation can influence B cell migration, differentiation into antibody-secreting plasma cells, and immunoglobulin class switching. This makes CB2 an attractive target for modulating humoral immunity in antibody-mediated diseases.
Further research into the endocannabinoid regulation of B cell responses and antibody production via CB2 may uncover opportunities for more targeted immune interventions.
The ECS's Homeostatic Role in Immunity
The endocannabinoid system (ECS) plays a critical role in maintaining homeostasis between the immune system and the body. The ECS helps regulate inflammation and modulate immune responses through its interactions with the endocannabinoids produced naturally within the body.
Modulating Inflammation and Immune Function
Research shows that the ECS can influence the proliferation, apoptosis, activation, and migration of various immune cells including T cells, B cells, and macrophages. By binding to cannabinoid receptors on these immune cells, endocannabinoids can alter cytokine production and either stimulate or suppress inflammatory responses.
This ability to fine-tune inflammation and immune cell activity highlights the ECS as a promising therapeutic target. Manipulating the ECS could potentially help treat inflammatory disorders like arthritis, bowel diseases, and even autoimmune conditions.
Maintaining Homeostatic Balance
The ECS helps the immune system respond appropriately to threats while also preventing excessive or chronic inflammation. This careful balance is what maintains homeostasis. The interplay between immune cells and endocannabinoids allows the body to mount defensive immune responses when necessary while also limiting these reactions to avoid unintended damage.
For example, endocannabinoids can limit inflammatory cytokine production by immune cells. This prevents excessive inflammation. However, if an infection occurs, the ECS can stimulate lymphocyte proliferation to ramp up the immune response. This flexibility to modulate immunity is key for health.
Future research should continue elucidating the intricacies of how the ECS communicates with the immune system. This could uncover innovative therapies that leverage the ECS to treat various immune and inflammatory disorders.
Endocannabinoids and Immune Cell Dynamics
Endocannabinoids play an important role in modulating immune cell function and movement. They influence cytokine production, chemotaxis, and the migration of inflammatory cells. One of their key effects is mediated through CB2 receptors found exclusively on immune cells.
Influence on Cytokine Induction and Immune Cell Migration
Studies show that endocannabinoids can modulate the induction of cytokines like interleukin-2 and interferon-gamma in T-lymphocytes. They also reduce the production of proinflammatory cytokines like TNF-alpha and IL-1beta by macrophages. This demonstrates their anti-inflammatory effects.
Additionally, endocannabinoids inhibit immune cell migration towards inflammatory stimuli. By regulating adhesion molecules and matrix metalloproteinases, they limit the infiltration of leukocytes into inflamed tissues. This restricts tissue damage induced by migrating immune cells.
Role of CB2 Receptors in B Cell Function
CB2 receptors are highly expressed in B lymphocytes and play a key role in their function. Activation of CB2 receptors inhibits B cell proliferation, differentiation into plasma cells, and immunoglobulin production.
Studies also show that CB2 receptor signaling in marginal-zone B cells of the spleen is important for their retention and survival. Since these cells rapidly produce natural antibodies against blood-borne antigens, CB2 receptors help maintain an effective first-line immune defense.
Therapeutic Potential of ECS Modulation
The effects of endocannabinoids on immune cell dynamics have promising therapeutic implications. Selective CB2 agonists that avoid psychotropic effects can potentially treat inflammatory and autoimmune conditions without causing immunosuppression.
Future research should explore opportunities for fine-tuning endocannabinoid tone to achieve controlled immunomodulation. This can pave the way for targeted ECS-based therapies.
Neurological and Immune Interactions via the ECS
The endocannabinoid system (ECS) plays an important role in regulating both neurological and immune functions in the body. Research has uncovered intricate connections between the ECS and the central nervous system, as well as between the ECS and immune cell dynamics.
Involvement of the ECS in Central Nervous System Processes
The ECS helps regulate various processes in the central nervous system including appetite, pain sensation, mood, and memory. Endocannabinoids act as neurotransmitters that bind to cannabinoid receptors throughout the brain and nervous system to modulate synaptic transmission. For example, a recent study found that endocannabinoids regulate the brain's response to stress in the nucleus accumbens. Given the ECS's role in neurological regulation, targeting the ECS has therapeutic potential for treating neurologic conditions. Modulating endocannabinoid tone could help manage symptoms or slow disease progression in conditions like multiple sclerosis, epilepsy, and neuropathic pain. More research is still needed to fully understand how best to leverage the ECS for neurological therapies.
Interconnectedness of Neurological and Immune Functions
There is growing evidence that the nervous and immune systems closely interact, with bidirectional communication mediated in part by the ECS. During inflammation in the central nervous system, endocannabinoids act as immune regulators to limit overactivation. For instance, microglial cells and astrocytes produce the endocannabinoid 2-AG in response to ATP release and purinergic receptor stimulation. This endocannabinoid release helps control inflammation during neuronal injury. The ECS also modulates T cell subsets and cytokine production, influencing neuroinflammatory versus neurodegenerative processes. Targeting the immuno-cannabinoid system could have therapeutic potential for both neurological and immune conditions. More research is still needed to elucidate the intricacies of this neurological-immune axis and how best to target it for therapies.
Therapeutic Implications
Given the evidence of ECS involvement in both neurological and immune regulation, targeting the ECS could have broad therapeutic implications. Treatments focused on modulating endocannabinoid tone or leveraging cannabinoid receptors may help manage symptoms or slow disease progression in conditions like MS, epilepsy, chronic pain, arthritis, inflammatory bowel disease, and more. However, more research is still needed to fully understand the complexities of the ECS in mediating neurological-immune interactions. Comprehensive studies focused on therapeutic targeting of the ECS for neurological versus immune disorders will help elucidate the best approaches for future therapies. END OF SECTION
Research Insights into ECS and Immune Response
The endocannabinoid system (ECS) plays a crucial role in regulating immune system function. Emerging research has illuminated the complex interplay between endocannabinoids and the innate and adaptive arms of immunity. Specifically, endocannabinoid tone has been shown to modulate immune cell proliferation, differentiation, apoptosis, and production of cytokines and antibodies. This highlights the immunomodulatory capacity of the ECS and its potential as a therapeutic target.
Impact on Innate and Adaptive Immunity
The ECS influences both innate and adaptive immunity in several ways:
- Regulates macrophage and dendritic cell function, including antigen presentation and cytokine secretion
- Modulates natural killer cell cytotoxicity and migration
- Influences T lymphocyte proliferation, polarization, and apoptosis
- Affects B cell antibody class switching and immunoglobulin production
Through these mechanisms, the ECS fine-tunes inflammatory responses, maintains immune homeostasis, and determines the balance between tolerance and immunity.
CB2 Receptor Targeting
The CB2 receptor, one of the main cannabinoid receptors, is expressed primarily in immune tissues. Targeting CB2 therefore represents a promising therapeutic strategy for modulating immune function. Key research insights include:
- CB2 activation dampens inflammatory responses and may be beneficial in autoimmune conditions
- CB2 signaling promotes regulatory T cell induction and self-antigen tolerance
- Selective CB2 agonists limit tissue damage in models of inflammatory disorders without psychoactivity
Thus, leveraging CB2 receptor signaling pathways could enable selective immune manipulation without affecting neuronal function.
In summary, advancing knowledge of ECS-immune interactions reveals new possibilities for targeting this system to treat immune disorders, while also highlighting the need for further research.
CB2 Receptor and B Cell Immunity
The CB2 receptor plays a key role in regulating B cell function and antibody production. Specifically, CB2 receptors are involved in modulating marginal zone B cells, a subset of B cells that produce natural antibodies and provide a first line of defense against pathogens.
Regulation of Marginal Zone B Cells
Research has shown that activation of CB2 receptors enhances the proliferation and survival of marginal zone B cells. This occurs through inhibition of the cAMP pathway and increased expression of anti-apoptotic proteins. As a result, CB2 receptor signaling promotes marginal zone B cell activation and differentiation into antibody-secreting cells.
Additionally, CB2 receptors regulate the migration and homing of marginal zone B cells. By modulating chemotaxis and cell adhesion molecules, CB2 receptors help direct marginal zone B cells to sites of inflammation and infection. This facilitates their interaction with pathogens and subsequent antibody production.
Natural Antibody Production
Marginal zone B cells are a key source of natural IgM antibodies - antibodies produced independently of pathogen exposure. CB2 receptor activation increases marginal zone B cell numbers and function, thereby bolstering natural IgM levels.
These natural antibodies provide early control of infections while the adaptive immune response develops. Hence, CB2 receptor-mediated marginal zone B cell regulation serves to enhance broad-spectrum immune protection through increased natural antibody production.
Therapeutic Prospects
The ability of CB2 receptors to modulate marginal zone B cell function and antibody responses presents opportunities for therapeutics. CB2 agonists could help boost antibody production in immunodeficiency disorders or restore marginal zone B cell numbers in conditions like age-related immunosenescence.
Additionally, selective CB2 modulation provides a means to enhance protective antibody responses without the psychoactive effects associated with cannabinoid CB1 receptor activation. Further research into CB2-targeted approaches may yield new immunomodulatory therapies.
Therapeutic Prospects Targeting the ECS
The endocannabinoid system (ECS) offers exciting potential for developing new treatments for immune disorders. By modulating the ECS through pharmacological agents that target cannabinoid receptors or enzymes involved in endocannabinoid metabolism, it may be possible to dampen harmful inflammatory responses or boost beneficial immune functions.
One especially promising therapeutic strategy involves selectively activating CB2 receptors. These receptors are found primarily on immune cells and appear to mediate several anti-inflammatory and immunosuppressive effects when engaged. CB2-selective drugs that avoid the psychoactivity caused by CB1 receptor activation could provide targeted immune modulation without causing cognitive impairment.
Potential Treatments Based on ECS Modulation
Some possibilities for ECS-based therapies include:
- CB2 agonists to suppress inflammation in conditions like arthritis, inflammatory bowel disease, multiple sclerosis.
- Inhibitors of endocannabinoid degradation to increase endocannabinoid tone and activate CB2 receptors.
- Combination therapies that incorporate CB2 activation along with other anti-inflammatory agents.
Such approaches leverage the ECS's natural role in immune regulation and homeostasis to therapeutic benefit.
Challenges and Opportunities
However, several challenges remain in exploiting the ECS for therapies:
- Difficulty of selectively targeting CB2 receptors while avoiding CB1 receptor effects.
- Lack of full understanding of the ECS's complex immunomodulatory roles.
- Ensuring therapies aimed at suppressing inflammation don't inadvertently increase infection risk.
Further research to elucidate the nuances of ECS signaling could uncover solutions and reveal exciting new opportunities for medicine. For example, optimizing CB2-selective drugs, identifying biomarkers to predict patient responses, and clarifying interactions with other biological systems.
In conclusion, the ECS holds significant promise as a target for innovating immune disorder treatments, but realizing its full potential will require overcoming current knowledge gaps through expanded research efforts.
Challenges and Future Research Directions
Despite the growing body of research on the link between the endocannabinoid system (ECS) and immune function, significant gaps in knowledge remain. Comprehensive studies focused specifically on targeting CB2 receptors for immune modulation are lacking. Further research is needed to fully elucidate the mechanisms by which endocannabinoids influence immune cell dynamics and to explore the therapeutic potential of leveraging the ECS to treat immune disorders.
Gaps in Understanding the ECS-Immune Connection
While endocannabinoids have been shown to affect immune cell proliferation, apoptosis, inflammatory cytokine production, and more, many questions persist regarding the intricacies of ECS signaling in immunity. The specific modes of action of endocannabinoids on various immune cell types and receptors require further characterization. Additionally, the complex crosstalk between the ECS and other modulatory systems influencing immunity is not yet fully mapped out.
Lack of Comprehensive CB2 Targeting Studies
To date, no large-scale clinical trials have been conducted to evaluate pharmacological targeting of CB2 receptors specifically for immunomodulation. Preclinical studies have demonstrated CB2 receptor agonists can dampen inflammatory responses, but comprehensive analyses are needed to assess the viability of CB2-directed therapies for immune disorders in humans. Safety, dosing, and potential side effects must also be thoroughly investigated.
Elucidating the Therapeutic Potential of the ECS
Harnessing the immuno-regulatory power of the ECS represents an exciting prospect for novel immunotherapies. However, realizing this potential will require extensive research into the effects of pharmacological modulation of endocannabinoid tone on innate and adaptive immune responses. Delineating the specific immunologic conditions that may be ameliorated via ECS targeting will help guide therapeutic development efforts going forward.
Future Research Directions
Clearly, the complex interplay between the ECS and immune system warrants much deeper investigation. Fruitful areas for future research include elucidating the impact of endocannabinoids on immunosenescence, characterizing ECS signaling defects in autoimmune conditions, and exploring combination therapies pairing ECS modulators with existing immunomodulatory agents. Such efforts will help unveil the full scope of possibilities for leveraging the ECS therapeutically to treat immune dysfunction.
The UK Perspective on ECS Research and Therapy
The status of endocannabinoid system (ECS) research in the UK is still in its early stages, but progressing steadily. A handful of universities such as Aberdeen, Reading and Ulster are exploring the therapeutic potential of cannabinoids and ECS modulation. However, limited funding and restrictive regulations have hindered more rapid advancements.
Regulatory Considerations for Cannabinoid-based Treatments
Cannabis is currently a Schedule 1 controlled substance in the UK, which impedes research due to extensive licensing requirements. The UK Home Office issues licenses for cultivation, possession and supply of cannabis for research purposes only under strict conditions. Researchers must demonstrate there are no viable alternatives to explore the research question. There are also complex regulations around cannabinoid-based medical products. The Medicines and Healthcare products Regulatory Agency (MHRA) is responsible for assessing safety, efficacy and quality of any cannabinoid-based medicine before approval. Only one cannabis-based product Sativex is currently approved for MS spasticity. The UK government is slowly recognizing the mounting evidence for medical cannabis. In 2018, medical cannabis was legalized but access has been extremely limited. The National Institute for Health and Care Excellence is currently developing guidelines for prescribing medical cannabis expected in October 2022.
Implications for Health Policy and Healthcare Integration
Several health policy groups in the UK such as the APPG for Medical Cannabis Under Prescription have called for reforms to improve patient access. Recommendations include allowing NHS prescriptions for medical cannabis and establishing a clear approval process via NICE. Many UK pain clinics and neurology centers are eager to integrate cannabis-based treatments but await more definitive guidance. Once ECS-modulating therapies obtain NICE approval, the treatments could be integrated into pain, neurology and immunology practices within the NHS system. The UK public is also increasingly receptive to harnessing the therapeutic potential of cannabis. A 2021 YouGov survey revealed 77% of Britons support legal access to medical cannabis. The UK government is responding through committees assessing reforms around medical cannabis laws and policies.
Conclusion and Implications for Health Policy
The research summarized in this blog post highlights the intricate link between the endocannabinoid system (ECS) and immune system regulation. The ECS plays a key role in modulating inflammation, immune cell activation, proliferation, apoptosis, and cytokine production. This positions the ECS as a promising therapeutic target for treating immune disorders.
In particular, the CB2 receptors found exclusively on immune cells have shown potential for selective immune modulation without psychoactivity. Targeting CB2 receptors could help regulate inflammation and antibody production in conditions like autoimmune diseases, allergies, and graft rejection.
As research continues to uncover the therapeutic prospects of the ECS, policymakers must consider updating regulations around cannabinoid-based treatments. Healthcare professionals should also stay abreast of advancements in ECS science and be prepared to integrate ECS-modulating therapies into patient care.
More comprehensive human trials are still needed to validate the safety and efficacy of therapies leveraging the immuno-modulatory effects of cannabinoids. However, the body of preclinical evidence covered in this blog provides reason for optimism.
In conclusion, research into the ECS-immune connection represents an exciting frontier in medicine. Policy changes and healthcare system readiness will be key to translating these scientific insights into tangible improvements in public health.


